I teach medical students about these, because most of them have never seen or heard of them.
ETA: because it keeps coming up and people keep making the same debunked claims, I am going to explain a few things, and I will try to keep things simple while explaining some of the more technical aspects.
𝟭. 𝗧𝗵𝗲 𝗖𝗢𝗩𝗜𝗗 𝘃𝗮𝗰𝗰𝗶𝗻𝗲𝘀 𝗮𝗿𝗲 𝗳𝘂𝗹𝗹𝘆 𝘁𝗲𝘀𝘁𝗲𝗱.
They used a staggered approach because of the need for the vaccine, but no corners were actually cut. They began phase 1, used the preliminary data to get approval to start phase 2 while they completed phase 1, then used preliminary data from phase 2 to get approval to start phase 3 while they finished phase 1 and 2. Each phase ran for the required amount of time, and the safety efficacy data was collected and analyzed. For getting through the regulatory process, instead of having to wait in the long queue and backlog of other clinical trials going on for other things that would delay the approval process, they were given priority and went to the head of the line for immediate review.
So yes, they were fully tested, from start to finish, and on patients who volunteered. A friend of mine was in the placebo arm of the trial—yes, these were double-blind randomized placebo-controlled trials.
𝟮. 𝗦𝗽𝗲𝗲𝗱 𝗼𝗳 𝘁𝗿𝗶𝗮𝗹𝘀.
It takes 10+ years for most drugs to be tested, get regulatory approval, and go to market for several reasons that were negated with the COVID vaccines.
Most drug trials:
• Have to recruit a very specific patients that have the condition being treated, but because of how generalized COVID is to the whole population, it was much easier to recruit patients.
• Cost a lot of money that needs to be raised, but money was made available through various grants and other means because of the urgent need to get a vaccine.
• Have to be run in sequence (i.e., finish one, start the next one), not parallel with a staggered start, but the COVID vaccines were run in a staggered parallel process as discussed.
• Have to wait in the queue of all of the other clinical trials that need to be reviewed by regulatory bodies, but the path was cleared to allow the review of the COVID vaccine trials to be at the front of the line for immediate review.
It’s also important to understand that the development of these vaccines didn’t start from scratch. A lot has been learned about coronaviruses since they were first identified in 1933, since they were first discovered in humans in 1965, and especially since SARS in 2003 and MERS in 2013 (among other coronavirus outbreaks that were contained). This research allowed us to know how to best target these viruses with vaccines.
mRNA technology has been in development for decades.
• mRNA was first identified in the 1961.
• Research on methods of delivering mRNA to cells began in 1978.
• The first use of mRNA for a vaccine was for the flu in mice in 1993.
• The first use of mRNA for a cancer vaccine in mice in 1995.
• The first use of the lipid delivery system for mRNA vaccines in mice was in 2012.
• The first clinical trial of mRNA as a rabies vaccine in 2013.
• The first use of the lipid delivery system for mRNA vaccines for the flu was in 2015.
The research on using mRNA for vaccines was decades in the making. When the pandemic hit, everything was in place for mRNA to be successfully used as a vaccine.
As for how the mRNA could be developed so fast, that’s a beautiful thing about science. From research on SARS, MERS, and other coronaviruses, we knew that the spike protein was the best thing to target with vaccines. As soon as someone had sequenced the gene for the coronavirus spike protein and published it online, everyone had access to it. That meant that researchers didn’t need to wait to get their hands on the virus for themselves, they could just take the available data and get to work. As a result, the work on a vaccine began in January 7 2020, barely a month after the first reported case of what became known as COVID.
𝟯. 𝗦𝗮𝗳𝗲𝘁𝘆 𝗽𝗿𝗼𝗳𝗶𝗹𝗲𝘀 𝗮𝗻𝗱 𝗹𝗼𝗻𝗴-𝘁𝗲𝗿𝗺 𝘀𝗶𝗱𝗲 𝗲𝗳𝗳𝗲𝗰𝘁𝘀.
We have to get into university-level biology and biochemistry courses, but I will try to keep it a simplified technical explanation. mRNA is not a stable, durable molecule. It got into the cells (which is also what happens with viruses) where the ribosomes translated it to make spike proteins. The mRNA might get translated a few times, but enzymes and chemical processes quickly degrade the mRNA (on the order of hours or days, and though fragments of the mRNA might be detectable longer, they aren’t able to be translated into proteins).
In a quick side note, there is something in biology known as the central dogma that discusses the direction of information flow in cells. DNA is transcribed to make RNA (which gets further processed to make mRNA or other RNA-based molecules and biomolecular machinery, but I am trying to keep things simple here, so let’s just focus on the mRNA). RNA is then translated into proteins. Proteins don’t become RNA, and RNA doesn’t become DNA (there are exceptions under very specific settings that aren’t relevant here, and I am trying to keep things simple). That means that once the RNA is gone, it’s not doing anything. The RNA is not changing the makeup of your DNA.
Once the cells make these spike proteins, they get processed and sent to the membrane of the cell. Through various processes, those spike proteins along with other proteins end up coming back into the cell. After they end up in the cell, they get cut up into small sequences of amino acids (the building blocks of proteins), get packaged onto another protein, and that protein goes to the cell membrane where it presents those fragments for immune cells (aka white blood cells, though it’s more nuanced than this, but again, keeping things simple). The immune system then recognizes that something is wrong inside the cell, treats the cell like it is infected, and kills the cells to stop what it thinks is a virus before a virus would have more time to replicate.
The whole process takes only a matter of days. Because of this, we know that any effects are going to show up in a few days, but just to be safe, they follow for a few months to check both for how effective the vaccine is at stopping an infection as well as preventing a severe infection, and for any side-effects and long-term effects.
𝟰. 𝗪𝗵𝘆 𝘃𝗮𝗰𝗰𝗶𝗻𝗲𝘀 𝘄𝗼𝗿𝗸.
Every vaccine ever created was not and is not 100% effective. Ideally, vaccines will be able to stop an infection before you know that you are sick. However, in order for your body to recognize that you have an infection, your cells have to get infected (it’s a bit more complicated with antibodies also playing a role in stopping an infection, but they aren’t always successful). Once your cells get infected, the same thing happens that I talked about in the section on the mRNA vaccine process (which, incidentally, is also why mRNA vaccines are good for your training your immune system because they mimic viral infection processes that other types of vaccines don’t always do). Your body is then able to fight the infection.
This is also why vaccines are important. By getting vaccinated, you are training your immune system to recognize the virus quicker and more effectively and eliminate it quicker. The virus gets into your cells and starts replicating, and your immune system spots this and responds, but because it takes time to fully mount a response, the virus replicates and can be transmitted (this is why with most infections, you can transmit the virus before you realize that you are even sick). But if you have been vaccinated, your immune system can respond much quicker with a more targeted response and clear the infection before the virus has much chance to replicate. This is why no vaccine is completely able to stop all infection and transmission, but they do reduce that considerably.
However, everyone’s immune system is a bit different. Some people have a more robust response than others. Some people will have a strong enough response that they never know when they get infected after being vaccinated. A much smaller number of people will come down with a mild case that resolves quickly with little transmission to others. An even smaller number will have a severe case with higher amounts of transmission (but looking at it statistically, this percentage is far less than people who aren’t vaccinated). And a very small number of vaccinated people can still die, but that is a very small number of people.
𝟱. 𝗕𝗼𝗼𝘀𝘁𝗲𝗿𝘀 𝗮𝗻𝗱 𝗲𝗳𝗳𝗲𝗰𝘁𝗶𝘃𝗲𝗻𝗲𝘀𝘀 𝗼𝗳 𝘃𝗮𝗰𝗰𝗶𝗻𝗲𝘀.
We don’t entirely know why our immune system has such a variation in response to infections.
For example:
• I have a friend who gets whooping cough pretty much every year. She has been vaccinated several times, and her body does fight off the infection, but her immunity is gone by the next year and she goes through it all over again.
• Prior to SARS-CoV-2 and COVID, there were six types of coronavirus that were circulating in society. If you caught one of those, you would clear it, be immune to it, but that immunity would wane over a few months, meaning that you could get sick with that same virus all over again.
• If you catch chickenpox, your body will mount a much more durable response that can last for decades, but it typically wanes with time and you can get shingles if your immunity drops too low and the virus re-emerges in your body. Normally, this waning isn’t a concern until in your 60s (which is when you should get vaccinated for shingles), but it can happen a lot earlier (for example, I am well under 60 and had shingles a year ago, my younger sister had shingles a few years before I did, and a friend had it in her 20s).
• Smallpox and measles infections tended to convey life-long immunity, but not always.
Another thing in this is the mutation rate of viruses. Some viruses mutate much faster than others, which makes it hard for your body to build up immunity to some types of viruses. This happens with flu viruses, coronaviruses, rhinoviruses, etc.
With highly successful vaccines like smallpox, polio, and measles, they are not 100% effective vaccines for everyone and they aren’t life-long:
• The smallpox vaccine is only about 95% effective in preventing severe infections. It is also only effective for 3–5 years (though partial immunity does last longer), but a booster shot brought that effectiveness higher and the duration of effectiveness went up to 20 years (lab workers who might get exposed to the virus get booster shots every 3 years).
• The polio vaccine is 90% effective at preventing paralysis after two doses, three doses takes that to 99–100% effectiveness, and a fourth booster takes that to essentially 100%. It’s not known how long the vaccine is effective for, but adults can get a 5th booster shot of they are at risk.
• The measles vaccine is about 93% effective at preventing symptomatic measles after one dose, and two doses brings that up to 97%. The effectiveness does decrease with time, and though most people don’t need it, some guidelines recommend to get a booster shot as an adult if you are at increased risk of exposure.
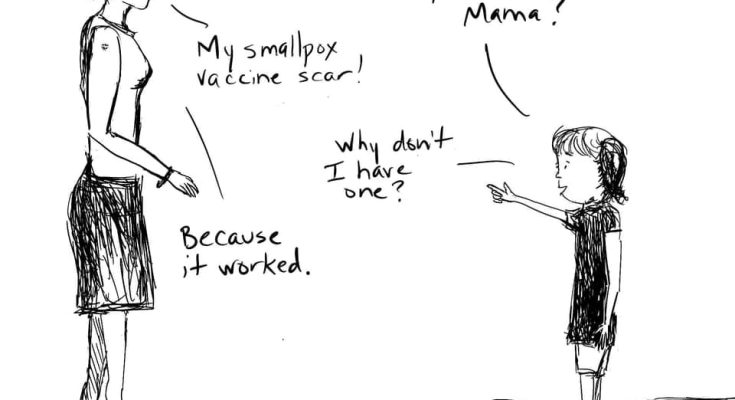
𝟲. 𝗘𝗿𝗮𝗱𝗶𝗰𝗮𝘁𝗲𝗱 𝘃𝗶𝗿𝘂𝘀𝗲𝘀
Vaccination campaigns are very successful:
• The last naturally occurring case of smallpox was in October 1977 (there was a lab exposure in 1978 of someone who was vaccinated as a child, though the particulars of how she was exposed is unknown, and she died). Smallpox now exists only in high security laboratories where it is preserved.
• We have eradicated two of the three wildtype strains of poliovirus. The last case of Wildtype 2 was in 1999 and the last case of Wildtype 3 was in 2012. In 2024, there were only 68 cases of Wildtype 1 in the world, but sadly, that is a big increase from the 12 in 2023. We are really close though!
• Rinderpest was a virus that infected even-toed ungulates like cattle, gaurs, buffaloes, large antelope, deer, giraffes, wildebeests, and warthogs. The last known case was in 2001. For a fun fact, it is believed that measles evolved from rinderpest.
Though it doesn’t involve a vaccination campaign, we have almost eradicated Guinea worm as well. In 2023, there were only 14 human cases and 878 animal cases, and in 2024, there were only seven confirmed human cases and 448 animal cases by November (these numbers are provisional and won’t be finalized until March 2025).
𝟳. 𝗧𝗵𝗮𝗹𝗶𝗱𝗼𝗺𝗶𝗱𝗲 𝗶𝘀 𝗮 𝗯𝗮𝗱 𝗮𝗿𝗴𝘂𝗺𝗲𝗻𝘁.
One, that happened 60+ years ago. Two, thalidomide is still used today for treating various diseases. Three, it was the regulatory system that blocked the approval of using thalidomide for morning sickness in the USA that saved countless babies. And four, a lot has changed in the regulatory approval process for pharmaceuticals, both as a result of lessons learned from the thalidomide scandal and from other scandals over the years.
While the regulatory process still has some problems, it is so much better than it was in the 1950s when they used thalidomide for morning sickness.
𝟴. 𝗖𝗹𝗮𝗶𝗺𝘀 𝗼𝗳 𝗼𝘃𝗲𝗿-𝗿𝗲𝗮𝗰𝗵.
In Canada, we have rights and freedoms guaranteed in the Canadian Charter of Rights and Freedoms. The very first section of the Charter states “The Canadian Charter of Rights and Freedoms guarantees the rights and freedoms set out in it subject only to such reasonable limits prescribed by law as can be demonstrably justified in a free and democratic society.” This means that restrictions can be placed on rights and freedoms in the case of things like a pandemic that is killing millions of people and overwhelming healthcare systems.
A history lesson about smallpox might be important as well. In addition to the vaccination campaigns, there were rigid and enforced quarantine orders for sick people or possibly sick people who were in contact until smallpox was eradicated, and this will again be the case is smallpox ever re-emerges. The vaccine campaign included compulsory vaccinations in some places, including under enforcement by police and this was declared constitutional. You didn’t get a choice in it.
We don’t do these kinds of public health enforcement measures anymore, but if a far more dangerous virus emerges in the future, we might see these things happen again.
𝟵. 𝗪𝗵𝘆 𝘆𝗼𝘂 𝘀𝗵𝗼𝘂𝗹𝗱 𝗴𝗲𝘁 𝘆𝗼𝘂𝗿 𝗳𝗹𝘂, 𝗖𝗢𝗩𝗜𝗗, 𝗮𝗻𝗱 𝗼𝘁𝗵𝗲𝗿 𝘃𝗮𝗰𝗰𝗶𝗻𝗲𝘀.
A lot of people reading this are likely young and healthy, and wonder why they should bother getting their annual flu and COVID vaccines. They figure that if they catch these, they might be sick for a few days but otherwise be okay (I used to think this too). Chances are high that this is true for them. But what about everyone around you? If you’re sick, who else are your spreading it to that might not be healthy and could end up really sick or dying?
This is the idea of herd immunity. If you’re vaccinated, even if you do happen to get sick, your immune system should be able to neutralize the virus a lot quicker. That means likely you will be sick for a shorter amount of time, have a milder case, and the really important part is that you will transmit much less virus to other people.
Getting vaccinated means that you are protecting your friends and family as much as you are protecting yourself. That’s why you should get vaccinated, and it’s why I get my flu and COVID vaccines every year. In order to achieve herd immunity, we need a certain percentage of the population to be vaccinated. This rate varies from disease to disease; for measles, we reached herd immunity around 95% of people vaccinated; for polio, we needed about 80% of people to be vaccinated; and for COVID, it’s estimated to be about 85%, but we aren’t certain.
𝟭𝟬. 𝗔𝗱𝘃𝗲𝗿𝘀𝗲 𝗲𝘃𝗲𝗻𝘁𝘀 𝗳𝗼𝗹𝗹𝗼𝘄𝗶𝗻𝗴 𝘃𝗮𝗰𝗰𝗶𝗻𝗮𝘁𝗶𝗼𝗻.
A lot of people like to go to the VAERS database and make all kinds of claims about the stuff reported in there. There are several reasons why this is not a useful argument.
The problem is that any event can get reported there, even when it has nothing to do with vaccines (e.g., car accidents, bald spots, nosebleeds, getting injured playing sports, incontinence, messed up hair dye, etc.). Even well-known and expected effects of vaccines are reported in the database as adverse events, including pain at the injection site, headaches, fever, chills, and fatigue. These all add to the total number of adverse events in the VAERS database.
The reporting also doesn’t have to demonstrate causal relationships, only correlation. For example, statistics are that between 10–20% of known pregnancies end in miscarriages. If you take 100 pregnant women at random, you can expect 10–20 of them will have a miscarriage. If you give all 100 of these women a vaccine, you can still expect that 10–20 women will have a miscarriage, but all of those could be reported as adverse events in databases like VAERS. The adverse event might have been caused by an underlying medical condition, by a medication or drug taken at the same time, or simply by chance, but we aren’t able to tell this just based on VAERS reporting.
Anyone, including non-healthcare professionals, can report, and there is a lot of unverified information, and in many cases, there is insufficient information in the reports that would be necessary to make an expert assessment of what caused this adverse event. Someone could even report a false event or report an event without having received a vaccine in the first place.
That is why VAERS is very clear that the reports in their database are not documentation that a vaccine caused the event and that the reports may include incomplete, inaccurate, coincidental, and unverified information. This is not to say that we should ignore VAERS. VAERS is a valuable early warning system, and it can be a really useful tool for detecting connections between diseases and adverse reactions and detect new, unusual, or rare reactions to vaccines, but we have to be aware of the problems with just grabbing numbers and not actually looking at what they mean.
It’s the same thing with adverse events reported from the COVID vaccine clinical trials. As a part of the reporting for the trials, every adverse event was tracked and reported, even if they had nothing to do with the vaccine. For example, a 72-year-old male developed cardiac arrhythmia after he was struck by lightning 28 days after being vaccinated, and this was included in the report as part of the total adverse events.
We should also look at the claims of increased risks of adverse events following COVID vaccinations. VAERS was helpful as an early warning system that a subset of the population were experiencing adverse events following vaccination. But it is important to understand what the normal background rate of the adverse event is, what the rate is following vaccinations, and the rate following infection if they are not vaccinated.
For example, one paper reported a 3x increase in cerebral venous sinus thrombosis following vaccination for COVID, but how does this compare to unvaccinated people who get COVID? The background rates are 1.3-2.0 per 100 000 person-years for the general population prior to COVID, the cases following COVID vaccination are 2.59 per 100 000 person-years, and the rates in unvaccinated are 83.3 per 100 000 person-years This means that hospitalizations due to cerebral venous sinus thrombosis with SARS-CoV-2 infection compared with those who received mRNA SARS-CoV-2 vaccination was 32.1 times higher.
𝟭𝟭. 𝗧𝘆𝗽𝗲𝘀 𝗼𝗳 𝘃𝗮𝗰𝗰𝗶𝗻𝗲𝘀.
A lot of people say that vaccines are made of viruses, but this is only partially accurate. There are actually several different types of vaccines:
• Inactivated vaccines (an inactive/dead virus that can’t replicate)
• Live-attenuated vaccines (a live/active virus, but one that is weakened or from a closely related virus that is too weak to get you sick but enough to trigger your immune system)
• Subunit, recombinant, polysaccharide, and conjugate vaccines (these are parts of a virus, such as proteins and sugar structures found in vaccines • Toxoid vaccines (some bacteria produce toxins, such as tetanus, and these use an essentially harmless version of the toxin to train your immune system)
• Viral vector vaccines (similar to mRNA vaccines, but instead uses a modified virus to deliver the RNA)
• Messenger RNA (mRNA) vaccines (what we are talking about in several areas here in this post)
Smallpox was a live-attenuated virus vaccine that used a related virus called vaccinia that wouldn’t cause smallpox but would train your immune system to recognize smallpox.
𝟭𝟮. 𝗥𝗲𝗳𝗶𝗻𝗶𝗻𝗴 𝘁𝗵𝗲 𝗱𝗲𝗳𝗶𝗻𝗶𝘁𝗶𝗼𝗻 𝗼𝗳 𝘃𝗮𝗰𝗰𝗶𝗻𝗲.
A lot of people like to point to how the CDC website changed the wording of how they defined vaccines as proof that the mRNA vaccines were not real vaccines. The definition originally on the CDC site said “a product that stimulates a person’s immune system to produce immunity to a specific disease,” and was changed to “a preparation that is used to stimulate the body’s immune response against diseases.”
From a physiological perspective, these are essentially the exact same thing, but the second one is more accurate. In order for you to develop immunity to a specific virus, you have to stimulate your immune system to respond against that type of virus. A vaccine simply is the way that you give knowledge of what a pathogen (e.g., virus) looks like in advance of you ever encountering that pathogen in the wild. The updated wording is more nuanced and aligns with what was discussed in earlier sections of this post (e.g., that no vaccine is 100% effective at totally blocking infection), but this refinement didn’t change the definition in any fundamental way.
𝟭𝟯. 𝗛𝘆𝗴𝗶𝗲𝗻𝗲, 𝘀𝗮𝗻𝗶𝘁𝗮𝘁𝗶𝗼𝗻, 𝗮𝗻𝗱 𝗻𝘂𝘁𝗿𝗶𝘁𝗶𝗼𝗻 𝗱𝗶𝗱𝗻’𝘁 𝗲𝗿𝗮𝗱𝗶𝗰𝗮𝘁𝗲 𝘀𝗺𝗮𝗹𝗹𝗽𝗼𝘅, 𝗮𝗻𝗱 𝗶𝘁 𝘄𝗮𝘀𝗻’𝘁 𝗼𝗻 𝘁𝗵𝗲 𝗱𝗲𝗰𝗹𝗶𝗻𝗲 𝘄𝗵𝗲𝗻 𝘁𝗵𝗲 𝘃𝗮𝗰𝗰𝗶𝗻𝗲 𝘄𝗮𝘀 𝗶𝗻𝘁𝗿𝗼𝗱𝘂𝗰𝗲𝗱.
Smallpox has been around for thousands of years. There are a range of dates for when it first emerged as a zoonotic infection from rodents in Africa, likely beginning with sporadic cases around 68,000 years ago, and fully diverged as a separate virus infecting only humans by around 10,000 years ago. Descriptions from India suggest it was there around 8500 HE/1500 BCE, and evidence on the mummy of the Egyptian pharaoh Rameses V suggests that he died from smallpox in 8846 HE/1145 BCE. Over the years, smallpox outbreaks happened in various areas and the virus was spread from community to community, and it killed roughly 1 in 3 people who caught it. Herd immunity could not develop on a global scale because new children are born and become new hosts susceptible to infections.
The first idea of something like vaccination was a technique called variolation, which emerged around 11000 HE/1000 CE in China. This technique involved collecting and crushing dried scabs or pus from infected individuals who had mild cases, and these mixtures were then scratched into the skin of another person or blown into their nostrils. Smallpox normally spread through droplets where it infected the upper airways before spreading to the rest of the body, but by inoculating the skin, the infection usually minor and remained localized, but it conveyed immunity. It wasn’t an entirely safe procedure, as people did develop symptoms of smallpox and approximately 1–2% of people who received variolation died following the procedure, compared to 30% who caught smallpox without having variolation. The technique spread from there to parts of India and Africa, but wasn’t introduced in Europe until the 1700s.
What we now know as the smallpox vaccine was first tested in 1796. English physician Edward Jenner noticed that milkmaids seemed to be protected from smallpox, and he realized that cowpox was the reason why. Milkmaids would get infected with cowpox, be mildly sick for a few days, then thereafter be protected from smallpox. This was a much safer form of variolation, as cowpox infections were much more mild than the infections from variolation with smallpox scabs.
Jenner decided to test this idea. Medical research ethics are much different today, as Jenner’s methods would not be acceptable in any sense today. He took matter from a cowpox sore on the hand of milkmaid Sarah Nelmes and scratched it into the skin of an 8-year-old boy named James Phipps (he needed someone who had not had either cowpox or smallpox for his test to be effective). Phipps was sick for a few days but recovered. Jenner then injected Phipps with smallpox six weeks later, and Phipps did not get sick. By 1801, testing had shown that inoculation with cowpox was an effective vaccine for smallpox and was much safer than variolation for the patient and the general public. Variolation was banned in England in 1840 in favour of vaccination.
At the time, miasmas were thought to be the cause of diseases. These “bad airs” were believed to be toxic gases emerging from decaying organic matter and carried seeds/spores of diseases (this is why plague doctors wore masks with bird-like beaks they would stuff with pleasant-smelling herbs and why public parks in towns and cities became a thing to provide clean air). It wasn’t until the late 11850s HE/1850s CE that Louis Pasteur conclusively demonstrated the germ theory of disease (though others before him had built up a body of knowledge to demonstrate the existence of microbes and had proposed they played a role in diseases before his experiments). Pasteur built on Jenner’s work
As rates of vaccinations increased, the rates of infection with smallpox went down, but there were still regular outbreaks and huge surges in cases among the unvaccinated. High rates of vaccinations in some areas had resulted in the eradication of smallpox in some areas by as early as 1900, but it wasn’t until 1958 that a global eradication plan was developed with international partners, and this program was intensified in 1967. Efforts included door-to-door vaccination drives, and outbreaks in places could be ended in a matter of weeks through these intense vaccination rates. The last natural case of smallpox was in 1977, and smallpox was declared eradicated in 1980.
Public health awareness, improved hygiene and sanitation, and access to better nutrition did help reduce the number of cases. But these were not sufficient to eradicate smallpox—vaccines are what was responsible for this incredible accomplishment.
𝟭𝟰. 𝗔𝗱𝗱𝗲𝗻𝗱𝘂𝗺: 𝘃𝗮𝗰𝗰𝗶𝗻𝗲𝘀 𝗮𝗻𝗱 𝗮𝘂𝘁𝗶𝘀𝗺.
The paper that reported a connection between autism and vaccines had been withdrawn and completely discredited along with its author. The author also lost his medical license for the incredibly unethical and inappropriate things he did around the paper. Study after study has shown absolutely no connection between vaccines and autism.
On a more humorous, tongue-in-cheek note, it’s more likely that autism causes vaccines. Autistic people are over-represented in research fields. Researchers are responsible for creating vaccines. There is a high likelihood that autistic people are helping to create vaccines. Which is why people joke that autism causes vaccines.
On a personal note, I am autistic. I am disgusted by how many people seem to think that it would be better for me to have died in my childhood from a preventable disease than to grow up and live a life that I enjoy. Vaccines did not cause my autism—I was born this way.
I teach medical students about these, because most of them have never seen or heard of them.